Summary
Future pandemics could be far worse than Covid-19. An Aotearoa Centre for Disease Control (CDC) would significantly enhance national capability to address such threats and collaborate with similar global efforts. It would build the science capacity needed for pandemic preparedness and response and for managing multiple ongoing infectious disease challenges. A key responsibility would be building integrated surveillance systems, coordinated diagnostic laboratory services, and a suitably skilled and trained workforce.
This organisation would be more effective, and make better use of resources, if it functioned as a ‘distributed’ centre with a hub providing core services and sector coordination, plus specialist nodes across universities and other organisations. Much of the resources already exist, with an established Crown Research Institute (ESR), and groups of expert infectious disease researchers and practitioners across the country. This Centre would coordinate and integrate these efforts to improve long-term health security in Aotearoa New Zealand, the Pacific, and globally.
The Covid-19 pandemic has had an enormous impact on health and the economy in Aotearoa NZ (NZ) and globally.1,2 Future pandemics are inevitable with multiple drivers of pathogen spillover from animals to humans—which is recognised as having been the main cause of emerging infectious diseases with pandemic potential.3 We also live with the threat of future pandemics that could be far worse than Covid-19.4 And these risks seem likely to increase with bioweapon development from advances in biotechnology and artificial intelligence, and further deterioration of the global geopolitical environment.4
NZ and the world in general are still far from adequately prepared to face such threats. The organisation of national infectious disease science capacity will no doubt be considered by the NZ Covid-19 Royal Commission which is due to report later in 2024. But at present NZ is an outlier in not having a dedicated national Centre for Disease Control (CDC). This omission contributed to NZ’s relatively low pandemic preparedness rankings prior to 20205 and presented additional challenges when NZ needed to coordinate an effective and complex emergency response at the onset of the Covid-19 pandemic. Although NZ’s response was broadly effective, it was not perfect.6 There were infrastructure and workforce issues, inequitable outcomes, and some costly failures (see appendix).
In this Briefing, we make the case for NZ to establish a national CDC with an initial focus on infectious diseases. ‘CDC’ is a working title only (see appendix).
How does NZ compare internationally?
In the decades leading up to the Covid-19 pandemic, many territories were strengthening their national infectious disease science capacity. A notable example was Taiwan which formed its CDC in 1990. This capacity proved valuable in their subsequent management of SARS and later Covid-19. Taiwan arguably had the most proactive Covid-19 response of any jurisdiction and launched the earliest pandemic response outside mainland China.7
Many countries have also been strengthening their public health workforce training for decades, but NZ is notably absent from the list of those with field epidemiology training programmes. These programmes ensure a capable workforce of epidemiologists ready to spring into action to track and limit the spread of emerging infectious diseases.8
In the wake of the Covid-19 pandemic, most countries are reviewing their core public health science infrastructure. Australia is working to establish a national CDC to improve its response to public health emergencies. It is also merging major communicable disease research centres in Melbourne (including the Doherty Institute for Infection and Immunity and the Burnet Institute) to form the Australian Institute for Infectious Diseases.
There are several NZ initiatives and proposals that could contribute to the proposed Centre. MBIE is leading Te Ara Paerangi – Future Pathways – a multi-year programme to build a future-focused research, science, and innovation system. A new infectious disease platform Te Niwha (hosted by ESR and the University of Otago) is now operating to support greater research capacity in this area. And in the 2023 budget, Government proposed establishing a Pandemic Response Centre (as part of the proposed Wellington Science City) to build better linkages between Crown Research Institutes and Universities.
What is a distributed CDC?
The essential feature of an Aotearoa CDC is that it would have responsibility for an integrated set of critical public health goals and functions. We outline these more fully in the Appendix below.
With this Centre, the whole is very much greater than the sum of the parts. It will integrate and coordinate multi-disciplinary functions such as surveillance, laboratory services, outbreak investigation, and the expertise to guide responses to improve control and prevention.
This Centre can also be seen as an infrastructure project. Achieving the necessary capacity will require consistent, long-term investment in core systems, services, and workforce. This capacity building goes well beyond simply funding short- and medium-term projects and research.
We have added the description ‘distributed’ to emphasise the benefits of building into this model an explicit focus on supporting defined nodes across the country which would be responsible for specific functions, best managed in certain settings. Obvious examples would be clinically focussed areas such as infection control, and developing prevention and control guidelines for particular categories of infections. This model also recognises that some areas of infectious disease research have well established organisational support already, such as the Food Safety Science and Research Centre and Immunisation Advisory Centre.
The Centre would have a regional and global perspective, which is critical given the worldwide distribution of pandemics and other major threats. It would be well-positioned to support regional health and development goals in the Pacific. There would be mutual value in the Centre working closely with the Australian CDC and other international organisations.
Benefits and challenges of a distributed CDC
There are multiple societal benefits of having an Aotearoa CDC including:
- Better preparedness and response to pandemic threats
- Improved prevention and management of ongoing (endemic) infections
- Improved health equity
- Improved efficiencies from more coordinated services and disease prevention
- Greater progress in science and innovation
- Improved long-term reliability of response capacity and trusted science advice
We describe these benefits, as well as potential challenges, in more detail in the appendix below.
Conclusion
An Aotearoa CDC will ensure NZ is better prepared for and able to respond to pandemic threats. It would also improve prevention and management of ongoing (endemic) infectious diseases. The potential benefits are large, long-term gains in population health, equity, and economic efficiency.
What’s new in this Briefing
- We need to plan for future pandemics – which may be more severe than Covid-19.
- NZ is an outlier in lacking a central science organisation dedicated to preparing for and responding to pandemics and endemic infectious diseases.
- NZ has much of the infectious disease science expertise, but lacks coordinated and consistent investment in essential infrastructure and workforce.
- The Government has announced that a ‘Pandemic Response Centre’ will be established as part of investment into science infrastructure in Wellington.
Implications for policy and practice
- NZ should establish an Aotearoa Centre for Disease Control (CDC) that can focus on both pandemic preparedness and control of all infectious diseases.
- Making this a ‘distributed’ centre, with some functions managed by well-defined nodes, could improve both effectiveness and efficiency.
Author details
Prof Michael Baker, Director, Public Health Communication Centre, and Department of Public Health, University of Otago Wellington
Prof John Crump, Professor of Medicine, Pathology, and Global Health, Co-Director, Centre for International Health, University of Otago Dunedin
Assoc Prof Amanda Kvalsvig, Senior researcher, Department of Public Health, University of Otago Wellington
Prof Jemma Geoghegan, Webster Family Chair of Viral Pathogenesis, Department of Microbiology and Immunology, University of Otago.
Assoc Prof Sir Collin Tukuitonga, Faculty of Medical and Health Sciences, University of Auckland; Director Centre for Pacific and Global Health; President, New Zealand College of Public Health Medicine
Dr Maia Brewerton (Ngāti Porou, Ngāti Kahungunu), Clinical Immunologist, Auckland and Waitemata Hospitals, Te Whatu Ora; Clinical Immunology and Allergic Diseases Team Leader at the Malaghan Institute
Dr John Kerr, Science Lead, Public Health Communication Centre, and Department of Public Health, University of Otago Wellington
Prof Nick Wilson, Co-Director, Public Health Communication Centre, and Department of Public Health, University of Otago Wellington
Appendices and additional detail
Historical context
New Zealand briefly had a New Zealand Communicable Diseases Centre (NZCDC), formed in 1989 from the previous National Health Institute (founded in 1954). This was a specialised unit, within the then Department of Health. It combined laboratory and epidemiological capacity for the first time in New Zealand, modelled on the US Centers for Disease Control and Prevention (CDC) [Dr Martin Tobias, personal communication]. It was disestablished in 1992 as part of a major health sector reorganisation that created the Ministry of Health and Crown Health Enterprises. The infectious disease functions were transferred to the Institute of Environmental Science and Research Ltd (ESR), one of the new Crown Research Institutes. The Ministry of Health then contracted ESR to provide these infectious disease services for the sector.
NZ’s Covid-19 response
The Covid-19 pandemic demonstrated that NZ can deliver an effective response to a global health emergency.6 Its small size gave it the advantage of having multiple informal links across its science and policy sectors allowing it to mobilise specialised workforce support, though often relying on large amounts of gifted time. This response was far from perfect, especially when contrasted with better prepared countries such as Taiwan.7 It also did not achieve equitable outcomes for Māori and Pacific Peoples.9 Its delivery was more costly and disruptive than it needed to be, and had expensive failures that more operational research might have helped to prevent.10 It could also have contributed more effectively to regional and global health security in a range of ways.
Infection disease capacity and infrastructure provided by an Aotearoa CDC
The proposed Centre provides several major advantages over current arrangements. Its organisational goals would be high-level, long-term responsibility for infectious disease prevention and control and pandemic preparedness and response, in collaboration with other sector agencies. It would have responsibility for building and maintaining sector capacity. In particular, integrated and highly functional surveillance and testing infrastructure and a highly skilled and networked workforce. These capacities include the following:
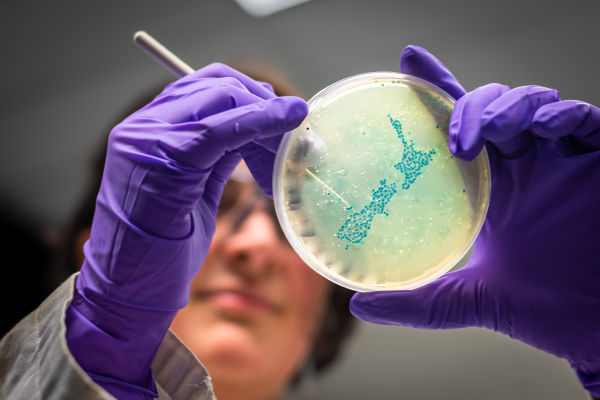
- Surveillance, laboratory, and response capacity – Critical infrastructure for managing both endemic and epidemic diseases include integrated surveillance, diagnostic testing, and contact tracing systems. Other critical capabilities include whole genome sequencing (WGS), disease modelling, infectious disease prevention and control expertise, and pandemic response capabilities.
- Workforce capacity – The science capacities needed for responding to infectious disease threats are specialised, multi-disciplinary, and also must represent cultural diversity and the needs of marginalised groups. This workforce requires strategic development, coordination, and investment through planning, training activities, and information dissemination. This Centre could facilitate movement between clinical, research, and operational roles and provide job security and a career structure to retain a core workforce with essential infectious disease expertise needed for responding to both endemic and pandemic infectious disease threats.
- Effective partnership with Māori and at-risk populations – The Centre will need to establish an effective Treaty Partnership and have health equity as a core goal. It should actively monitor health equity across the infectious disease sector, identify practical ways to minimise and eliminate inequities, support Māori and Pacific leadership, build community partnerships, and co-design public health initiatives with Māori, Pacific Peoples, and other under-served groups.
- Effective partnerships with international and global centres and bodies – The Centre would have a regional and global perspective, which is critical given the worldwide distribution of pandemics and other major threats. It would be important to support regional health and development goals and pandemic preparedness and response in the Pacific, particularly in the realm nations (Cooks Islands, Niue and Tokelau). There would be mutual value in the Centre working closely with the Australian CDC and other international centres.
- Effective public communication and education – The Centre could take a supporting role in disseminating accurate information to the public, helping to mitigate misinformation and promote public health measures.
- Science advocacy for supportive policy, legislation, and resources – The Centre could play a crucial role in advising policymakers on measures needed for infectious disease prevention and control, and preparedness and response to pandemics. This function includes recommendations on public health policies, border biosecurity, vaccination strategies, legislation, and resources to support the necessary capacities and responses within NZ and the wider Pacific region.
- Addressing research, evaluation, and development needs – The Centre would be well-placed to identify and fund strategic areas for research investment within NZ. Such areas would include operational research aiming to rapidly evaluate and improve the quality of critical services. This function could include helping to identify core research capabilities for NZ and fostering international collaborations.
Improved outcomes from an Aotearoa CDC
An adequately resourced Aotearoa CDC with a strong mandate could achieve major advances in the following areas:
- Better preparedness and response to pandemic threats – The Centre would be focussed on emerging infectious disease threats, including preparedness and the ability to rapidly scale up an effective response. It could also support an ‘all-of-government’ response by modelling, scenario planning, simulation exercises, and running outbreak and pandemic training exercises. Given its regional and global focus, these benefits would apply beyond NZ.
- Improved prevention and management of ongoing (endemic) infectious diseases – Endemic infectious diseases cause a large burden of acute disease, long-term effects, and healthcare costs.11 Improved measures to prevent such infections would also improve pandemic capacity and vice versa.12 Several current infectious disease problems have been highlighted in the Briefing this year, including the rising incidence of Strep A infections13, congenital syphilis14 and meningococcal disease.15 These problems are largely preventable with a well-coordinated, evidence-informed response.
- Reduced health inequities – Effective responses to pandemics, particularly if excluded entirely (a form of elimination), are likely to support improved health equity. Better prevention and control of infectious diseases should also improve health equity as these diseases have much higher rates for Māori and Pacific Peoples, and those living in more deprived areas.11 In low and middle-income countries, infectious disease inequalities are far more extreme than in NZ. The CDC could support programmes to address such inequities, particularly in the Pacific region.
- Improved efficiency and cost-effectiveness – The Centre could improve efficiencies by ensuring highly coordinated and integrated infrastructure. It could also draw on expertise across the health and research sectors as required by helping to break down institutional silos between universities, CRIs, and research centres and promote cooperative work. It could also be a major point of contact for liaison and information sharing with the new Australian CDC (which could achieve multiple gains, including service delivery in highly specialised areas, improved knowledge sharing, and quality assurance). It would also link with other key centres across the Asia-Pacific region and globally.
- Greater progress in science and innovation – The focus of the CDC would link science to applied research challenges. It would also create a highly multidisciplinary environment which would foster innovation.
- Improved long-term reliability of response capacity and trusted science advice – The CDC could be organised to ensure consistent long-term capacity building and operation partially protected from government sector reorganisations. Its governance and accountability arrangements could also ensure sufficient independence to maintain its position as a trusted source of scientific advice. These benefits are important to safeguard the long-term thinking needed for responding to severe and catastrophic risk.16
Potential costs and challenges in forming an Aotearoa CDC
NZ already has most of the essential resources to form a distributed CDC, notably a CRI that provides many of the key components at a national level (ESR), public health expertise across the health system, and leading scientists and practitioners across universities and research organisations. There would still be challenges to establishing and operating an effective CDC:
- Ensuring sufficient resources – The distributed CDC would require additional resources for its establishment and to address current gaps in capacity. Ultimately, it would generate savings by improved coordination of services and reductions in healthcare demand.
- Establishing a clear mandate – The prevention and control of infectious diseases is a major government responsibility, with key agencies including the Ministry of Health (and Public Health Agency), Te Whatu Ora (including the National Public Health Service), and Te Aka Whai Ora all having active roles in strategy and service delivery. It would be necessary to define the delegated responsibilities of this Centre, accountabilities, and governance arrangements. The role of the distributed CDC would be a significant expansion of the infectious disease activities currently provided by ESR, particularly the sector leadership and coordination functions. Examples of these critical functions are listed in Table 1, and summarised here:
- Infectious disease prevention and control sector capacity development and coordination (1, 2, 3, 4, 5)
- Global health intelligence including pandemic risk assessment (6)
- Integrated epidemiological and laboratory-based surveillance (7, 8, 9, 10)
- Laboratory services and capacity development (10, 11, 12, 13)
- Outbreak investigation and response (14, 15)
- Pandemic preparedness, including disease modelling, simulations, training (16, 17, 18, 19)
- Workforce training, development, and support (20, 21)
- Infectious disease prevention and control guidelines (22)
- Coordinated development of critical science areas (23, 24, 25, 26, 27, 28, 29)
- Operational research and quality improvement (30)
- Research on critical prevention and control capabilities, in collaboration with sector (31, 32, 33, 34)
Scope of an Aotearoa CDC
The initial focus of this Centre would be on infectious diseases as there is ample evidence supporting this need. The description of a distributed Aotearoa Centre for Disease Control (CDC) is just a working title for discussion. It would need further development to reflect its eventual role and identity. The US CDC for example was renamed as the Centre for Disease Control and Prevention to reflect that its focus included a strong emphasis on prevention, as well as controlling existing health threats
One question that needs further discussion is around the potential value of including veterinary infectious diseases within its scope. There is potential value of incorporating New Zealand's national veterinary laboratory service which is part of the Ministry of Primary Industries. The National Animal Health Laboratory in Wallaceville is co-located with ESR laboratories allowing some shared use of facilities. Doing this would be consistent with adopting a One Health approach which is particularly useful for considering zoonotic diseases and emerging infectious diseases at the animal-human interface.17
There are other public health areas which would also benefit from greater coordination and use of translational science, including environmental health, injury prevention, public health emergencies generally, and long-term conditions. This broader focus is seen internationally, notably in the US CDC and the proposed Australian CDC.
Table 1: Examples of critical functions for infectious disease (ID) prevention and control that would be provide by a distributed Aotearoa CDC. This list also illustrating the potential split between a central hub and specialised nodes and areas where collaboration with Australia and other international centres could be highly beneficial*
P = Primary responsibility, PP = Potential primary responsibility, C = Active collaboration
|
Critical functions
|
Centre Hub
|
Decentralised Nodes
|
- Strategic planning for ID prevention and control, including capacity development
|
P
|
C
|
- Infectious disease science sector coordination
|
P
|
C
|
- Active collaboration with Australian CDC, Pacific Region, WHO and international partners on capacity development*
|
P
|
|
- Equity lens on all strategic and operational issues
|
P
|
C
|
- Māori partnership and co-design of systems
|
P
|
C
|
- Global health intelligence including emerging IDs, pandemic risk assessment*
|
P
|
|
- Surveillance systems development and operation
|
P
|
C
|
- Epidemiological analysis, reporting, and communication
|
P
|
PP (specific areas)
|
- Contact tracing systems development and operation
|
P
|
C
|
- Laboratory diagnostic system coordination and integration
|
P
|
C
|
- Specialist diagnostic (reference) testing*
|
P
|
PP (specific areas)
|
- Whole genome sequencing (WGS)*
|
P
|
PP (specific areas)
|
- Biobanking (culture collection)
|
P
|
C
|
- National outbreak investigation and response support
|
P
|
C
|
- Local outbreak investigation and response support
|
P
|
C
|
- Disease modelling and pandemic simulations*
|
P
|
PP
|
- Pandemic preparedness policy for Aotearoa*
|
P
|
PP
|
- Pandemic preparedness policy support for Pacific*
|
P
|
PP
|
- Pandemic response emergency support
|
P
|
C
|
- ID workforce training, development, and support*
|
P
|
PP
|
- Information dissemination and networking with sector
|
P
|
C
|
- Infectious disease prevention and control guidelines*
|
P
|
PP (specific areas)
|
- Vaccine assessment and delivery science support
|
P
|
PP
|
- Border biosecurity science support*
|
P
|
PP
|
- Indoor air quality and respiratory disease science support
|
P
|
PP
|
- Infection control science (including masks) support
|
P
|
PP
|
- Antimicrobial resistance (AMR) science support*
|
P
|
PP
|
- Food and water borne (enteric) disease science support
|
P
|
PP
|
- One Health, ecology, and zoonoses science support*
|
P
|
PP
|
- Operational research, evaluation, and quality improvement
|
P
|
PP
|
- Research on ID determinants and risk factors
|
P
|
PP
|
- Research on vaccine development and production (eg. collaboration with Australia on mRNA technology)*
|
C
|
PP
|
- Research on ID therapeutics*
|
C
|
PP
|
- Research on ID diagnostics*
|
C
|
PP
|
*Areas where international collaboration, particularly with Australia, would be critical to support service delivery in highly specialised areas, improve knowledge sharing, and provide quality assurance
https://www.phcc.org.nz/briefing/why-we-need-aotearoa-centre-disease-control-cdc