References
- Immunisation Advisory Centre. Recommended and funded vaccines during pregnancy. Cited 18 March 2024. Available from: https://www.immune.org.nz/factsheets/recommended-and-funded-vaccines-during-pregnancy
- Health New Zealand Te Whatu Ora. Immunisation Handbook 2024 Version 1. Cited 18 March 2024. Available from: Immunisation Handbook 2024 Version 1 – Health New Zealand | Te Whatu Ora
- Institute of Environmental Science and Research Limited. Pertussis Dashboard. Cited 18 March 2024. Available from: https://www.esr.cri.nz/digital-library/pertussis-dashboard/.
- McIntyre PB, Best E, Byrnes CA, et al. Pertussis deaths in New Zealand without community transmission—an infant immunity gap? The Lancet Regional Health - Western Pacific 2023; 37:100850.
- Meijer WJ, van Noortwijk AG, Bruinse HW, et al. Influenza virus infection in pregnancy: a review. Acta Obstetricia et Gynecologica Scandinavica 2015; 94(8):797-819.
- Duque J, Howe S, Azziz-Baumgartner E, et al. Multi‐decade national cohort identifies adverse pregnancy and birth outcomes associated with acute respiratory illness hospitalisations during the influenza season. Influenza and other respiratory viruses 2023; 17:e13063.
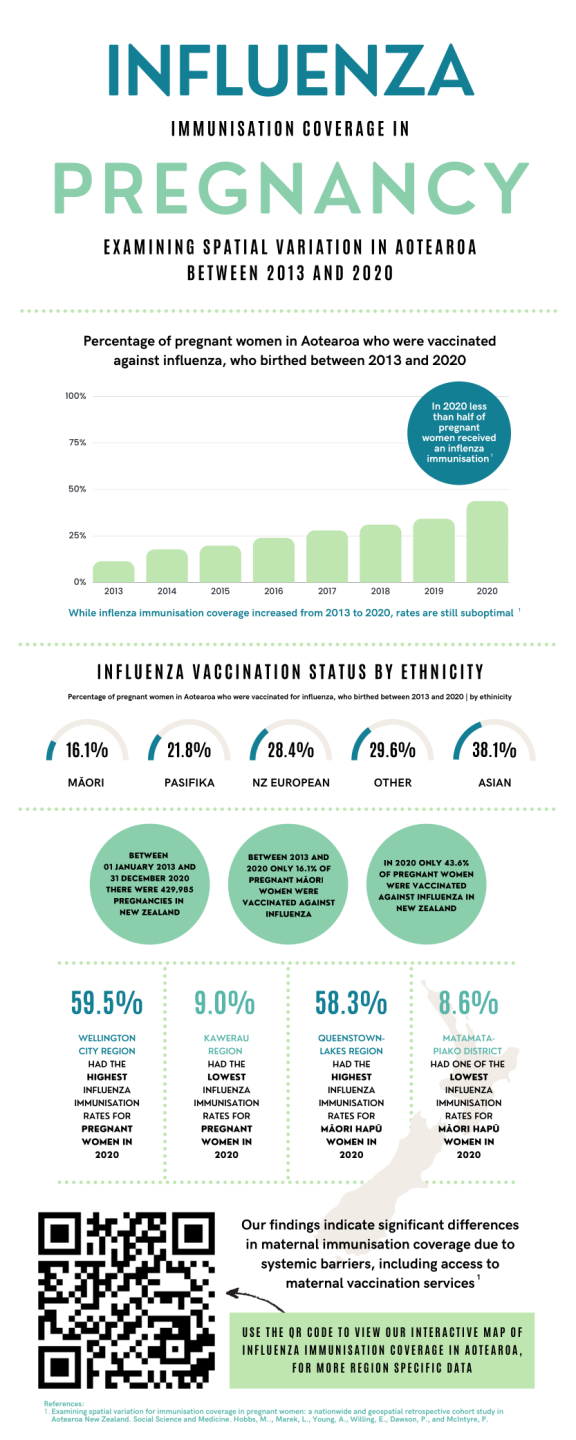
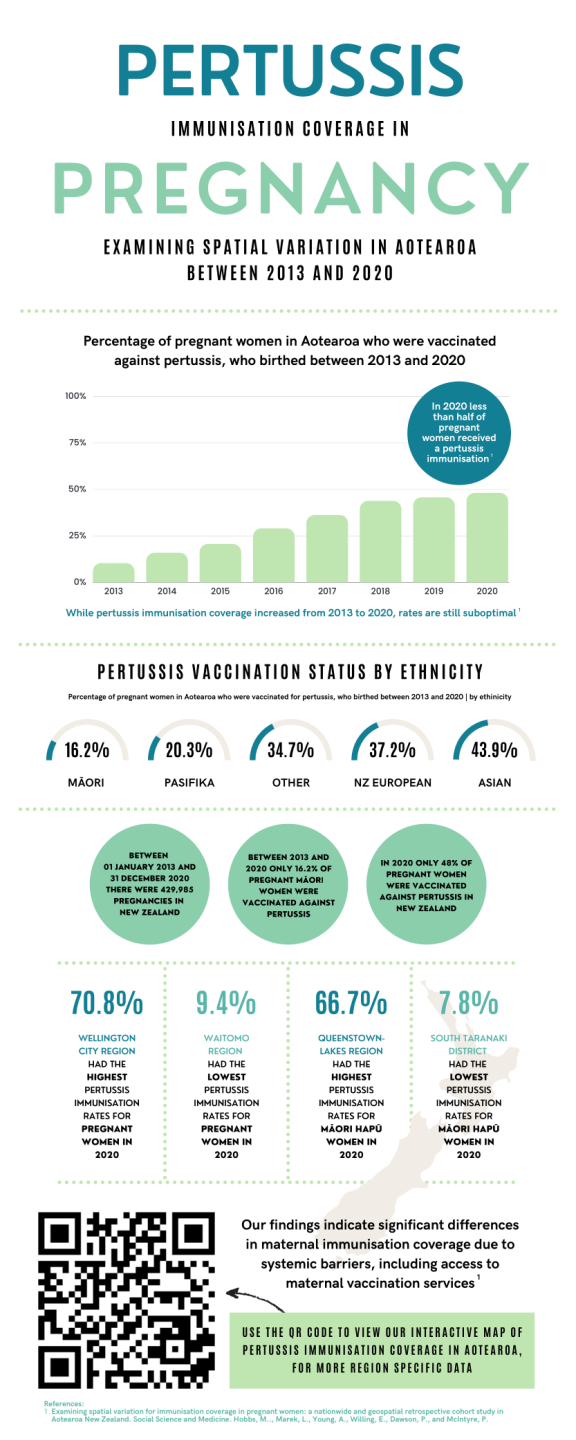
- Pointon L, Howe AS, Hobbs M, et al. Evidence of suboptimal maternal vaccination coverage in pregnant New Zealand women and increasing inequity over time: A nationwide retrospective cohort study. Vaccine 2022; 40(14):2150-60.
- Hobbs M, Marek L, Young A, et al. Examining spatial variation for immunisation coverage in pregnant women: A nationwide and geospatial retrospective cohort study in Aotearoa New Zealand. Social Science & Medicine 2023; 335:116228.
- Marek L, Hobbs M, Wiki J, et al. Spatial-temporal patterns of childhood immunization in New Zealand (2006–2017): an improving pattern but not for all? European Journal of Public Health 2021; 31(3): 561-66.
- Marek L, Hobbs M, McCarthy J, et al. Investigating spatial variation and change (2006–2017) in childhood immunisation coverage in New Zealand. Social Science & Medicine 2020; 264:113292.
- Makowharemahihi C, Lawton BA, Cram F, et al. Initiation of maternity care for young Maori women under 20 years of age. New Zealand Medical Journal 2014; 127(1393): 52-61.
- Gauld N, Martin S, Sinclair O, et al. Influences on Pregnant Women's and Health Care Professionals' Behaviour Regarding Maternal Vaccinations: A Qualitative Interview Study. Vaccines 2022; 10(1): 76.
- Young, A, Willing E, Gauld N et al. Midwives’ perceptions of enablers and barriers to pertussis and influenza vaccination in pregnancy and information sharing. New Zealand College of Midwives Journal 2023; 59:29-38.
- Jeffreys M, Ellison-Loschmann L, Irurzun-Lopez M, et al. Financial barriers to primary health care in Aotearoa New Zealand. Family Practice 2023; doi.org/10.1093/fampra/cmad096
- Gauld NJ, Braganza CS, Babalola OO et al. Reasons for use and non-use of the pertussis vaccine during pregnancy : an interview study. Journal of Primary Health Care 2016; 8(4):344-50.
- Young A, Charania NA, Gauld N, et al. Informing women about maternal vaccination in Aotearoa New Zealand: Is it effective? Midwifery 2023; 120:103636.
- Young A, Charania NA, Gauld N, et al. Knowledge and decisions about maternal immunisation by pregnant women in Aotearoa New Zealand. BMC Health Services Research 2022; 22:779.
- Sharp M. Covid-19 vaccines: DHB criticised Ministry of Health for rollout delays, warns of flourishing conspiracy theories. Cited 18 March 2024. Available from: https://www.stuff.co.nz/national/health/coronavirus/124684983/covid19-vaccines-dhb-criticised-ministry-of-health-for-rollout-delays-warns-of-flourishing-conspiracy-theories.
- Macredie F, Willing E, Dawson P et al. Interventions to improve vaccine coverage of pregnant women in Aotearoa New Zealand. Journal of Primary Health Care 2023; 15(3):230-37.
- Frew PM, Zhang S, Saint-Victor DS, et al. Influenza vaccination acceptance among diverse pregnant women and its impact on infant immunization. Human Vaccines and Immunotherapeutics 2013;9(12):2591-602
- Willing E. Hitting the target without missing the point: New Zealand's immunisation health target for two year olds. Policy Studies 2016; 37(6):535-50.
- Tenbensel T, Chalmers L, Willing E. Comparing the implementation consequences of the immunisation and emergency department health targets in New Zealand: A tale of two targets. Journal of Health Organization and Management 2016;30(6):1009-24.
- Irurzun-Lopez M, Pledger M, Mohan N et al. "Closed books": restrictions to primary healthcare access in Aotearoa New Zealand - reporting results from a survey across general practices. New Zealand Medical Journal, 2024; 137(1591):11-29.
About the Briefing
Public health expert commentary and analysis on the challenges facing Aotearoa New Zealand and evidence-based solutions.
Subscribe

Public Health Expert Briefing
Get the latest insights from the public health research community delivered straight to your inbox for free. Subscribe to stay up to date with the latest research, analysis and commentary from the Public Health Expert Briefing.