Summary
Antenatal depression affects about 20% of pregnant women/wāhine globally, increasing pregnancy complications and postnatal depression. Psychotherapy is recommended but is often inaccessible due to cost, time, and stigma. Antidepressants are advised for severe cases, but only 3% of pregnant wāhine in Aotearoa use them, often due to infant health concerns. Poor nutrition during pregnancy is linked to higher maternal depression.
Our research showed that additional micronutrients (vitamins and minerals) during pregnancy for the treatment of symptoms of antenatal depression improved birth outcomes and may mitigate depression’s negative effects. These results highlight potential healthcare savings and the need for policy development to improve diets and prescribe micronutrients during pregnancy, especially for low-income New Zealanders.
The data also suggest the need to consider improving nutrition in pregnancy (e.g., vouchers for whole foods), and for consideration around the routine promotion or prescribing of micronutrient supplements by the NZ Government and relevant professional groups.
This Briefing discusses outcomes from a new observational study of birth outcomes in mothers who struggled with symptoms of antenatal depression and were treated with micronutrients. We discuss the importance of the findings with respect to cost savings, guidelines, and implications for nutrient prescribing.
Current treatments for antenatal depression: Are they enough?
Globally, antenatal depression affects 21% of pregnant wāhine worldwide.1 Untreated antenatal depression is linked to higher rates of adverse birth outcomes and complications, such as preterm birth, lower birth weight, poorer newborn health (lower Apgar scores), and a greater need for interventions.2-5 These adverse outcomes can negatively affect infants’ early health and development, with lasting physical and mental health impacts into adulthood.6 7
Psychotherapy is a recommended treatment, but access barriers like cost, time, and stigma often prevent its use.8 Antidepressants are advised for severe cases as the benefits outweigh potential risks which are deemed to be of little clinical significance.9 However many pregnant people stop taking antidepressants, often due to worries about how they might affect infant health.10 Only 3-6% of pregnant wāhine in Aotearoa take antidepressants,11,12 despite the prevalence of depression being much higher.
These limitations have sparked interest in nutritional interventions, which are gaining recognition for their role in supporting mental health during pregnancy.13 This is where the NUTRIMUM trial steps in.
The NUTRIMUM trial, conducted at Te Puna Toiora, Te Whare Wānanga o Waitaha, examined whether broad-spectrum micronutrients—a combination of vitamins and minerals—could offer a safer, effective alternative to antidepressants for treating symptoms of antenatal depression. NUTRIMUM was a 12-week randomised controlled trial (RCT) of micronutrients versus an active placebo, whereby the micronutrients outperformed the placebo in improving overall mental health outcomes.14 The RCT was followed with an observational study, recruiting other pregnant wāhine to help contextualise the effect of the micronutrients on birth outcomes.15
What did the observational phase of the NUTRIMUM Trial explore?
The observational follow up study included three groups:
- Micronutrient Group: Mothers taking micronutrients for at least eight weeks to treat symptoms of antenatal depression.
- Medication Group: Mothers using antidepressants during pregnancy to treat depression.
- Reference Group: Mothers not using the NUTRIMUM micronutrients or psychiatric medications.
What Were the Results?
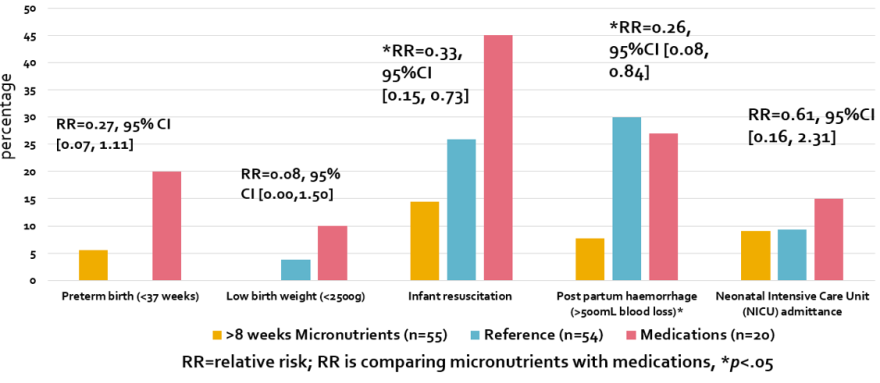
Key results are shown in Figure 1.
- Birth Outcomes Are Comparable to the Reference Group
Mothers taking micronutrients had birth outcomes similar to the Reference group, with no increased risks of preterm births, low birth weight, or delivery complications and on par or better than national averages in Aotearoa. The one significant group difference favoured a better outcome for the micronutrient-exposed infants, with significantly less bleeding after delivery (post-partum haemorrhage) in vaginal births (7.7% versus 30%). This means the risks conferred to the infant based on the mother’s history of depression were possibly mitigated by the micronutrients. - Micronutrients Outperformed Antidepressants
Compared to the Medication group, the Micronutrient group had significantly better results:- Average gestational age was longer (39.5 weeks vs 38.5 weeks)
- These infants were longer at birth (52.2 cm vs 50 cm)
- Rates of infant resuscitation were lower (14.5% vs 45%)
Duration of Use Matters
Longer exposure to micronutrients correlated with increased infant weight and length, indicating a potential dose-response effect.
Figure 1. Main birth outcomes across the three groups.
Source: Heaton et al. (2025)15
What about cost benefits?
The study points to a way to potentially reduce health care costs. Although the micronutrient supplement costs around NZ$200 per month in this study, the potential savings from improved birth outcomes could offset this expense. For example, the incremental costs of a late preterm birth (32-36 weeks) relative to a term birth are ~NZ$28,000.16 About 12% of wāhine in Aotearoa experience untreated antenatal depression,17 and the risk of a preterm birth for an untreated mother with depression is about 15%.18 With ~60,000 births per year, treating antenatal depression with micronutrients could save ~NZ$10.5 million per annual cohort. Even further savings could potentially arise if Pharmac negotiated a good deal for any approved supplement that could be prescribed in pregnancy.
What might this mean for health workers and policy in NZ?
The results of this study highlight the value of good nutrition in pregnancy. In some countries this is supported by Government-provided vouchers for real whole foods during pregnancy, which have led to improved outcomes for the offspring.19 Pregnancy is one of the most cost-effective times for any government to allocate its resources for prevention.20 Such voucher schemes could be pilot tested in Aotearoa.
The routine promotion or prescribing of micronutrient supplements could also be considered further by the NZ Government and relevant professional groups (Royal Australian and NZ Colleges of Psychiatrists and Obstetricians and Gynaecologists). The likely benefits (as per this and other studies) would need to be balanced with potential downsides e.g., those of:
- Risk of over-supplementation since excessive doses of fat-soluble vitamins (e.g., A, D, E, K) can accumulate in the body and harm the fetus (in particular, high vitamin A intake is associated with birth defects).
- The potential risk that pregnant wāhine may develop a false sense of security, relying on supplements while neglecting healthy eating patterns
If you are a health professional who works with people who are pregnant, it is worth discussing the potential benefits of a healthy diet in pregnancy21 as well as an additional micronutrient supplement for improving birth outcomes.
Although supplementation is not a replacement for nutritious food, these data illustrate the positive effect that additional nutrients can have on outcomes as proof of principle that the nutritional environment is inadequate for some pregnancies. Research and further replication could evaluate the potential cost savings through supporting birthing persons to eat more nutrient-dense foods during pregnancy, with supplementation as an additional support, on both mental and physical health outcomes.
What is new in this Briefing
- Currently, standard treatments for antenatal depression do not eliminate the risks associated with depression, such as preterm birth, low birth weight and the need for resuscitation at birth.
- The birth outcomes from the NUTRIMUM study show that supplementation with micronutrients to treat symptoms of antenatal depression was associated with gestational ages, weight, length, and rates of resuscitation on par or better than national averages and better than standard care (antidepressants).
- Micronutrient use was associated with lower rates of bleeding after delivery (post-partum haemorrhage) than typical pregnancies in Aotearoa.
Implications for policy and practice
- This study highlights that the nutritional environment is paramount to better outcomes for both the mother and offspring. If micronutrients were used in pregnancy as a treatment for antenatal depression, the cost savings for Aotearoa on improved birth outcomes could be in the millions of dollars per yearly cohort treated.
- There are currently no policies in place in Aotearoa for easy and affordable access to nutritious kai in pregnancy. Adopting such policies would align with the Ministry of Mental Health’s ambition to dedicate 25% of the Mental Health budget to prevention. Government policy overseas on providing vouchers for real whole foods during pregnancy have led to improved outcomes for the offspring.
- The routine promotion or prescribing of micronutrient supplements could also be considered further by the NZ Government and relevant professional groups (Royal Australian and NZ Colleges of Psychiatrists and Obstetricians and Gynaecologists).
Authors details
Prof Julia Rucklidge, School of Psychology, Speech and Hearing, Te Whare Wānanga o Waitaha | University of Canterbury
Jessic Heaton, School of Psychology, Speech and Hearing, Te Whare Wānanga o Waitaha | University of Canterbury
Dr Hayley Bradley, School of Psychology, Speech and Hearing, Te Whare Wānanga o Waitaha | University of Canterbury
Dr Siobhan Campbell, School of Psychology, Speech and Hearing, Te Whare Wānanga o Waitaha | University of Canterbury
Prof Elena Moltchanova, School of Mathematics and Statistics, Te Whare Wānanga o Waitaha | University of Canterbury
Dr Lesley Dixon, New Zealand College of Midwives, Christchurch
Prof Roger Mulder, Department of Psychological Medicine, Ōtākou Whakaihu Waka | University of Otago
Appendix
The study's limitations include small sample sizes, application only to mild-to-moderate depression, and varying exposure days to micronutrients during pregnancy. There was only a small percentage of Māori and Pacifica participants in NUTRIMUM (9%), and all participants identified as female, and therefore we do not know whether these results would extend across different ethnic groups and gender identification. Nevertheless, it is one of the largest controlled studies in pregnancy for the treatment of symptoms of antenatal depression and as such, is relevant to informing treatment guidelines.