References
- Te Whatu Ora | Health Zealand. Pertussis (whooping cough) 2024 [Available from: https://www.tewhatuora.govt.nz/for-health-professionals/clinical-guidance/immunisation-handbook/15-pertussis-whooping-cough/ accessed 20th June 2024].
- Institute for Environmental Science and Research (ESR). Pertussis Report. In: ESR, ed. Wellington, New Zealand: ESR, 2019.
- Ganeshalingham A, Reed P, Grant C, et al. Hospital costs of Bordetella pertussis in New Zealand children. New Zealand Medical Journal 2016; 129 (1445), 75 - 82.
- Somerville RL, Grant CC, Grimwood K, et al. Infants hospitalised with pertussis: estimating the true disease burden. Journal of Paediatrics and Child Health 2007;43(9):617-22.
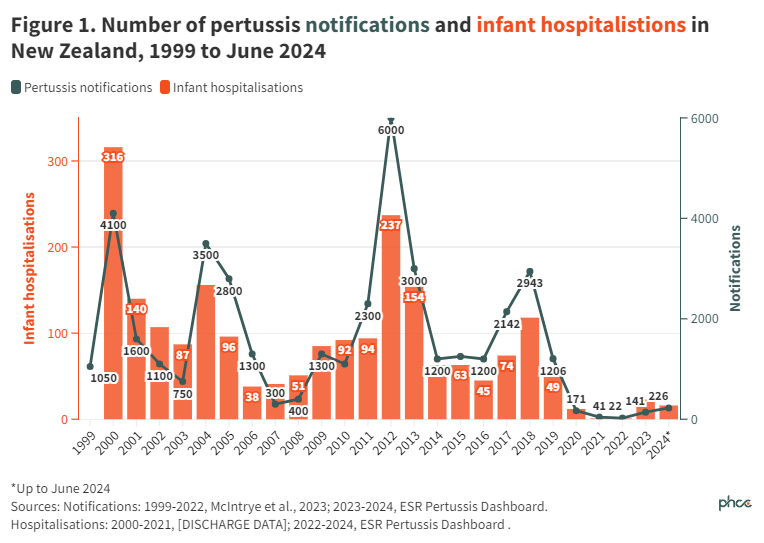
- McIntyre PB, Best E, Byrnes CA, et al. Pertussis deaths in New Zealand without community transmission—an infant immunity gap? The Lancet Regional Health–Western Pacific 2023;37
- Institute for Environmental Science and Research (ESR). Pertussis Dashboard 2024 [Available from: https://www.esr.cri.nz/digital-library/pertussis-dashboard/ accessed 20th June 2024].
- Nowlan M, Turner N, Kiedrzynski T, et al. Pertussis control strategies: A consistent approach for New Zealand Synopsis of Ministry of Health Workshop, April 2015. 2016
- Wan M, Zhang G, Yi H. Unraveling the resurgence of pertussis: Insights into epidemiology and global health strategies. Pulmonology 2024:S2531-0437 (24) 00055-2.
- Wiley K, Zuo Y, Macartney K, et al. Sources of pertussis infection in young infants: a review of key evidence informing targeting of the cocoon strategy. Vaccine 2013;31(4):618-25.
- Quinn HE, McIntyre PB. The impact of adolescent pertussis immunization, 2004-2009: lessons from Australia. Bulletin of the World Health Organization 2011;89(9):666-74.
- Te Whatu Ora | Health Zealand. Pregnancy Immunisation Coverage Infographic, 2024 (unpublished)
- Vygen-Bonnet S, Hellenbrand W, Garbe E, et al. Safety and effectiveness of acellular pertussis vaccination during pregnancy: a systematic review. BMC Infectious Diseases 2020;20:1-22.
- Public Health Communication Centre (PHCC). Protecting hapu māmā and newborn babies through immunisation during pregnancy in Aotearoa New Zealand: Public Health Communication Centre Aotearoa; 2024 [Available from: https://www.phcc.org.nz/briefing/protecting-hapu-mama-and-newborn-babies-through-immunisation-during-pregnancy-aotearoa-new accessed 20th June 2024].
- Makowharemahihi C, Lawton B, Cram F, et al. Initiation of maternity care for young Māori women under 20 years of age. The New Zealand Medical Journal 2014;127(1393)
- Te Whatu Ora | Health Zealand. Initial Priorities for the National Immunisation Programme in Aotearoa: Te Whatu Ora, 2022.
- Young A, Charania NA, Gauld N, et al. Informing women about maternal vaccination in Aotearoa New Zealand: Is it effective? Midwifery 2023;120:103636.
- Gauld NJ, Braganza CS, Babalola OO, et al. Reasons for use and non-use of the pertussis vaccine during pregnancy: an interview study. Journal of Primary Health Care 2016;8(4):344-50.
- Gauld N, Martin S, Sinclair O, et al. Influences on pregnant women’s and health care professionals’ behaviour regarding maternal vaccinations: a qualitative interview study. Vaccines 2022;10(1):76.
- Macredie F, Willing E, Dawson P, et al. Interventions to improve vaccine coverage of pregnant women in Aotearoa New Zealand. Journal of Primary Health Care 2023;15(3):230-37.
- National Centre for Immunisation Research and Surveillance (NCIRS). Sharing Knowledge About Immunisation: Pregnancy & Newborn Vaccinations Australia: National Centre for Immunisation Research and Surveillance Australia; 2024 [Available from: https://skai.org.au/pregnancy-and-newborn accessed 26th June 2024].
- Duckworth S. Immunisation for Pregnant Women: Audience research with pregnant women. Prepared for the Ministry of Health. Wellington, New Zealand: Litmus, 2015.
- Gauld N, Martin S, Sinclair O, et al. Mapping the maternal vaccination journey and influencing factors for Māori women in Aotearoa New Zealand: a qualitative study. Journal of Primary Health Care 2022;14(4):352-62.
- Hobbs MR, Morton SM, Atatoa-Carr P, et al. Ethnic disparities in infectious disease hospitalisations in the first year of life in New Zealand. Journal of Paediatrics and Child Health 2017;53(3):223-31.
- Allen + Clarke. Improving New Zealand’s childhood immunisation rates Evidence Review: Allen + Clarke, 2019.
- Nowlan M, Willing E, Turner N. Influences and policies that affect immunisation coverage-a summary review of literature. New Zealand Medical Journal 2019; 132(1501):79-88.
- Chan WC, Papaconstantinou D, Oulaghan B, Lee M, Anderson P. Immunisation Coverage (Primary Series) and Children’s Interactions with the Health System. Auckland, New Zealand: Te Whatu Ora Counties Manukau, 2021.
- PHARMAC. Decision on joint proposal with Health New Zealand to enable childhood vaccinations to be given in pharmacies 2024 [Available from: https://pharmac.govt.nz/news-and-resources/consultations-and-decisions/decision-on-joint-proposal-with-health-new-zealand-to-enable-childhood-vaccinations-to-be-given-in-pharmacies accessed June 2024].
- Proposal to allow pharmacists to provide childhood vaccinations: Radio New Zealand; 2024 [Available from: https://www.rnz.co.nz/news/national/508584/proposal-to-allow-pharmacists-to-provide-childhood-vaccinations].
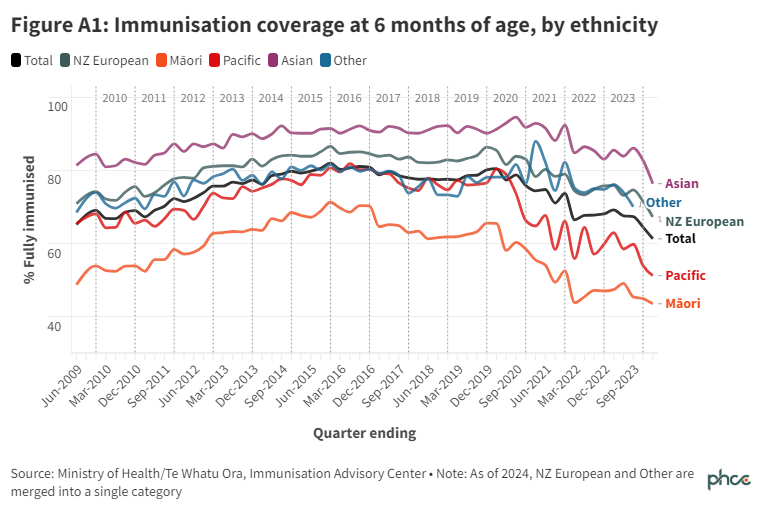
- Immunisation Advisory Centre. Immunisation coverage at 6 months of age, by ethnicity: Immunisation Advisory Centre; 2024 [Available from: https://reporting.immune.org.nz/#/immunisation-coverage-at-6-months-of-age-by-ethnicity accessed 20th June 2024].
About the Briefing
Public health expert commentary and analysis on the challenges facing Aotearoa New Zealand and evidence-based solutions.
Subscribe

Public Health Expert Briefing
Get the latest insights from the public health research community delivered straight to your inbox for free. Subscribe to stay up to date with the latest research, analysis and commentary from the Public Health Expert Briefing.