Summary
This Briefing summarises our recently published study that compares the 1918-19 influenza pandemic with the Covid-19 pandemic. It highlights similarities and differences in the nature of these pandemics, the responses, and their impacts on Aotearoa New Zealand and globally. It also emphasises the importance of learning from the past to inform current and future pandemic management, focusing on public health infrastructure, international cooperation, and addressing social determinants of health. The analysis reveals the critical role of rapid scientific advancements, such as new strategic approaches (notably elimination) and vaccine development, in mitigating Covid-19's effects. By extracting lessons from the 1918-19 influenza pandemic, we suggest ways to improve resilience and equity in healthcare systems for better preparedness and response to future public health emergencies.
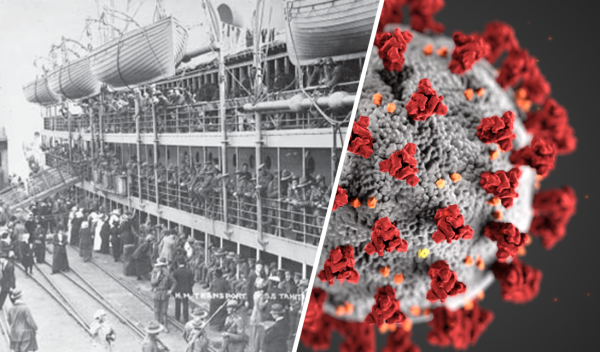
We recently published a study1 that explored the similarities and differences between the 1918-19 influenza pandemic and the Covid-19 pandemic. These pandemics share similarities in their global impact, exposing the fragility of societies to emerging pathogens. The influenza pandemic of 1918-19, occurring in the aftermath of the First World War (WW1), claimed an estimated 50-100 million lives worldwide,2 with a significant toll in Aotearoa New Zealand (~9,000 deaths), marking it as the country's worst recorded natural disaster (see Appendix).3
Fast forward a century, the Covid-19 pandemic, caused by the SARS-CoV-2 virus, emerged in late 2019, leading to millions of reported cases and deaths globally.4, 5 New Zealand, while faring better than most countries (Figure 1), still experienced major impacts on its health system, economy, and society.1
Figure 1: Excess mortality in six OECD jurisdictions: Cumulative number of deaths from all causes compared to projections based on previous years, per million people*
Both pandemics affected largely immunologically naïve populations, resulting in much higher health impacts than endemic infections (eg, seasonal influenza). However, differences in the viruses' characteristics, such as their transmission dynamics (eg incubation periods, reproduction numbers), and speed of evolution influenced the patterns and durations of the pandemics and respective responses. The rapid spread of the 1918-19 H1N1 pandemic virus, combined with the lack of effective vaccines, and limited public health interventions, resulted in a devastating mortality rate. However, a distinctive feature of the Covid-19 pandemic is the on-going occurrence of major waves for at least four years. The global scientific community’s ability to quickly develop Covid-19 vaccines has also been a defining difference, significantly reducing mortality and morbidity associated with the disease.
A further notable difference is mortality patterns, with a “w-shaped” age distribution observed during the 1918-19 influenza pandemic but not for Covid-19 (Figure 2).6, 7 Instead, Covid-19 mortality in New Zealand increased exponentially with age. An important similarity across these pandemics was the persisting health inequities seen for Māori, as manifest in significantly highly mortality rates than for the European population.3, 8
A major difference was the greatly enhanced ability to take a highly strategic approach to pandemic management for Covid-19 by using public health and social measures (PHSM) to eliminate the pandemic for a sustained period. This delay provided time for development and delivery of vaccines, antivirals and other measure that greatly improved health outcomes for New Zealand. These options were not available in 1918, although some countries were able to use PHSM to exclude influenza entry for sustained periods.9
Figure 2: Cumulative mortality rate (deaths per 1,000 population) in Aotearoa New Zealand during the 1918-19 Influenza Pandemic (for European-origin population) and during the Covid-19 pandemic up to 2023 (all ethnic groups), by age and sex*
Lessons from 1918-19 for the ongoing management of Covid-19
The 1918-19 influenza pandemic highlighted several key areas for improvement in pandemic preparedness and response that are relevant to managing Covid-19. It showed that pandemic preparedness and response needs to be adaptable to different agents. This preparedness also needs to be highly strategic and include elimination (and exclusion) as options along with suppression and mitigation as evidence suggests that delaying arrival of severe pandemics can offer large benefits.1, 10, 11
New Zealand's experience with the 1918-19 pandemic underscored the consequences of inadequate healthcare resources and access, particularly for Māori populations, who suffered disproportionately.3 This historical inequity has echoed through the Covid-19 pandemic, where Māori and Pacific peoples have faced higher rates of hospitalisation and mortality.12, 13
The rapid global spread of both pandemics underscores the need for international cooperation and timely sharing of information. The 1918-19 influenza pandemic's spread was facilitated by troop movements and post-WW1 migrations, while global passenger jet travel has played a similar role in the dissemination of SARS-CoV-2. Effective international collaboration and communication are essential for controlling the spread of disease and coordinating responses to public health emergencies.
The Māori response to Covid-19 showcased resilience and innovation. Māori health providers played a crucial role in outreach, testing, and vaccination efforts within their communities. For example, several iwi-initiated border controls for their respective areas, echoed the approaches used in 1918-19 by iwi to limit the spread and severity of disease and thus protect their whānau and communities.3, 14, 15
Moreover, the 1918-19 influenza pandemic demonstrated the critical role of community engagement and public adherence with health measures (Figures 3 & 4). The varied responses to social distancing, mask mandates, and vaccination campaigns during the Covid-19 pandemic have highlighted the need for clear, consistent communication and culturally appropriate public health strategies to ensure a successful response.
Figure 3: Medicine department at the Wellington Town Hall during the 1918 influenza epidemic ***
*** Shows where the standard mixture and tonic were prepared and bottled. Mrs. Waters (right) was in charge. Taken by an unidentified photographer. Reproduced from New Zealand Free Lance: 1/2-C-016207-F, 1918, Alexander Turnbull Library: National Library of New Zealand, Wellington, New Zealand.
Figure 4: Workers at Kōkiri Marae preparing food and sanitation packages for the Lower Hutt and Wainuiomata communities during Covid-19 pandemic
Photo: Luke Pilkinton-Ching, University of Otago.
Implications for Future Pandemic Planning
The lessons learned from the 1918-19 influenza pandemic are valuable for refining current and future pandemic responses:
- Pandemic preparedness and response systems need to adapt to the features of different agents. They need to be able to take a highly strategic approach to risk assessment and management to take advantage of available PHSM, vaccines, and other technologies. An elimination strategy may be the optimal response for severe pandemics.11
- Pandemic resilience needs to focus on equity, particularly for Māori. This means addressing inequities in the social determinants of health including, housing, employment, and access to healthcare, which are essential for reducing vulnerabilities within populations.
- Health systems and public health infrastructure need to be strengthened to ensure they are resilient and capable of responding to surges in demand.
- There needs to be an international effort to build global pandemic management capacity, including strengthening the World Health Organization's role in coordinating global responses and key international agreements such as the International Health Regulations.16, 17
- There needs to be investment in research and development for PHSM, vaccines, therapeutics and other interventions. The rapid development of Covid-19 vaccines has saved millions of lives globally18 and thousands in New Zealand.19 It has also highlighted the importance of ongoing investment in medical research, including studying virus evolution and vaccine efficacy over time.
- Strengthening health systems and public health infrastructure to ensure they are resilient and capable of responding to surges in demand.
What is new in this Briefing?
- Comparisons between New Zealand's responses to the 1918-19 influenza and Covid-19 pandemics highlight important similarities and differences.
- Both pandemics show the need for robust healthcare and equitable access to improve future pandemic responses. For example, both pandemics caused persisting health inequities for Māori, as manifest in significantly higher mortality rates than for the European population.
- A major difference is the enhanced ability to take a highly strategic approach to pandemic management for Covid-19 by using public health and social measures (PHSM) to eliminate the pandemic providing time for development and delivery of vaccines, antivirals and other measure that greatly improve health outcomes.
Implications for public health
- Pandemic preparedness and response need to be adaptable to different agents.
- This preparedness needs to be highly strategic and include elimination (and exclusion) as options along with suppression and mitigation depending on the nature of the pandemic.
- There is a need for focused system-level action in public health policy and practice to better address the social determinants that create and sustain health inequities, including pandemic outcomes, and stronger health systems that ensure equitable access for all, including Māori communities.
- Effective pandemic responses depend on essential public health infrastructure and international cooperation in pandemic preparedness and response.
Authors details
Dr Jennifer Summers, Dr Matire Harwood, Dr Julie Bennett, Professor Michael Baker and Professor Nick Wilson
Acknowledgements:
This research was supported by a donation from the late Professor Richard Seddon of Otago University, New Zealand. We thank the New Zealand Ministry of Health/Manatū Hauora for providing additional Covid-19 data directly for the purposes of this briefing.
The authors declare no competing interests.
Further details:
ChatGPTv4 was used to summarise the authors’ original text from our peer-reviewed journal article. This article was then checked for accuracy and further developed.
* Figure 1 details: Source: Our World in Data, sourced from the Human Mortality Database (HMD) Short-term Mortality Fluctuations project and the World Mortality Dataset (WMD), Human Mortality Database, World Mortality Dataset. Note: The cumulative difference between the reported number of deaths since 1 January 2020 and the projected number of deaths for the same period based on previous years. The reported number might not count all deaths that occurred due to incomplete coverage and delays in reporting. Data extracted 3 January 2023.
** Figure 2 details: The 1918–19 pandemic mortality data cover the entire period of the pandemic in New Zealand and are reproduced from Summers JA 2013 and derived/approximated from publicly available sources from the New Zealand Official Year-Book, 1924. Mortality data from 1918–19 for the Māori population are not available; therefore, mortality rates are likely underestimates. Covid-19 mortality data cover the period of January 2020–December 31, 2023. Mortality data were provided by the New Zealand Ministry of Health/Manatū Hauora, and population totals were sourced from Stats NZ/Tatauranga Aotearoa. Death was classified as a Covid-19 death when Covid-19 was the underlying cause of death or a contributory cause of death. Deaths with no recorded sex (n=7) are not included.
Appendix:
1918-19 Influenza Pandemic in New Zealand: A Historical Disaster
The 1918-19 influenza pandemic largely unfurled in two waves in New Zealand. The first, milder wave occurred between July and October 1918, while the more deadly second wave swept the nation in November and December of the same year.3 The majority of pandemic-related deaths transpired during this second wave, which swiftly spread across the country. More than 9,000 influenza deaths were recorded, and this is likely an undercount.3 Some localised prevention measures, such as quarantine and travel restrictions, were implemented, but there was no coordinated public vaccination effort as no vaccine was available.3 The long-lasting impact of this new pandemic influenza strain persisted for several years, with documented long-term effects internationally.20, 21
The 1918-19 pandemic's impact on the Māori population was profound. The pandemic had a disproportionate impact on Māori, with an estimated 4% of the Māori population dying from pandemic influenza in the last two months of 1918,3 thus revealing underlying health disparities and barriers in healthcare access. Overcrowded living conditions, limited access to health care, and prevalent chronic diseases contributed to the high mortality rate.3 This pandemic exacerbated existing inequalities and brought to light the urgent need for improved public health measures and healthcare access for Māori.
The 1918-19 influenza pandemic also had a profound impact on New Zealand's children. They not only fell victim to the virus but many were also forced to assume caregiving roles for their families and communities, with many left orphaned.3 Additionally, there was a sudden drop in the country's annual birth rate in 1918 and more so in 1919, attributed to the interplay between influenza infections, social effects, and stillbirths/fetal loss.6, 22
Covid-19 in Aotearoa New Zealand: A Modern Challenge
The first case of Covid-19 in New Zealand emerged on 28 February 2020, ushering in a series of events, including border controls, the first national stay-at-home order ('lockdown'), and the implementation of comprehensive public health and social measures.23 The New Zealand Government initially adopted an elimination strategy, emphasising strict border control and rapid outbreak extinguishment.23 The Government responded with localised and national public health measures, including lockdowns. In late 2021, the Delta variant prompted a shift from the elimination strategy to a suppression strategy with the introduction of the Covid-19 Protection Framework.10, 23 However, this framework was retired in September 2022, leaving limited public health protections in place, which could be described as a mitigation strategy.10, 23, 24
New Zealand's pandemic plan, conceived in anticipation of an influenza pandemic and developed prior to Covid-19, has been scrutinised for its applicability to Covid-19, given the distinct characteristics of the latter.25 Despite these challenges, New Zealand achieved an overall decline in mortality, and an increase in life expectancy during the first two years of the Covid-19 pandemic.26 New Zealand has also experienced low estimates of cumulative excess mortality (-0.04% as of October 2023) compared to the pre-Covid period, unlike other high-income nations, such as the United States (11.6% - August 2023), United Kingdom (9.8% - October 2023), Australia (5.2% - June 2023), Japan (3.2% - August 2023) and Sweden (4.9% - August 2023) (Figure 1).5
The largest Covid-19 waves in New Zealand, driven by the Omicron variant and its sub-lineages, occurred in 2022.27 By the end of 2023, the country had reported a total of 3,645 Covid-19 deaths13 and was experiencing the fifth Covid-19 wave driven in part by the JN.1 variant (recently classified as a "variant of interest" by the World Health Organization).13, 28 Māori and Pacific populations faced (and still do so) a disproportionate burden of hospitalisations and deaths, coupled with lower vaccination rates in these groups.12, 13, 29